
Supporting Women Through Relactation
by Lucy Ruddle, IBCLC
Lucy Ruddle, IBCLC
Editor’s Introduction: Lucy Ruddle is an International Board Certified Lactation Consultant (IBCLC) who resides in the United Kingdom (UK). She’s a mother who has successfully relactated herself and runs a UK-based relactation Facebook group. She specializes in relactation and breastfeeding grief (which we all know often go hand-in-hand). If you’d like to learn more about Lucy, you can find her on Facebook here. She also has a fantastic blog where she’s published a wide array of lactation-related posts and resources.
Author’s note on language: Throughout this article, I refer to “Breastfeeding” however, I am aware that not everyone who lactates identifies with this specific term. The term “Chestfeeding” may be preferred – please do use whichever language you feel most comfortable with. I have used a broad range of terms such as Mother, Mum, she, they, person, parent etc. throughout this article. It is my aim to embody the diversity of language individuals relate to in the field of lactation.
It’s a bit of a mythical beast, relactation. It’s talked about across the parenting forums and Facebook groups around the world. It seems that barely an “I’ve stopped breastfeeding and I feel awful” post goes by without someone saying, “You know you can relactate, right?” And yet even in the field of lactation, practitioners aren’t always sure how to support parents asking them if it’s really possible to bring their milk back.
Let me start by saying a clear “YES”, relactation absolutely is possible. If humans can induce lactation, then, of course, they can produce milk after doing so once before. There are anecdotal reports of Grandmothers relactating to feed their grandchildren, and many of us are aware of the outstanding work currently happening to support refuges to rebuild milk supply so they can safely feed their babies.
However, what I often hear is women being told to “Just put baby to the breast.” Which seems very logical to be fair, so this may come as a surprise… “Just put baby to the breast” rarely works. I run a relactation group on Facebook and have relactated myself. Over the last 5 years, I have lost count of how many women I have supported through this process. I have also lost count of how many babies simply will not latch to an empty breast. These babies have been taking a bottle for at least a couple of weeks, and usually, they were exposed to one before mum stopped breastfeeding altogether. They are used to a silicone teat dripping or pouring a steady flow of milk straight down their throats. They rarely have the patience to play around with a breast which isn’t giving up the goods.
Of course, we should encourage mum to find out if baby will latch. Let’s be honest, a willing baby makes rebuilding milk supply a lot easier. BUT if baby won’t attach, and the adult keeps pushing the matter, then we are on a fast track to breast aversion. Let’s take this thing, breastfeeding, which is supposed to be connecting and lovely, and turn it into a battlefield, shall we? No. If baby doesn’t want to latch, then we drop the rope, as it were.

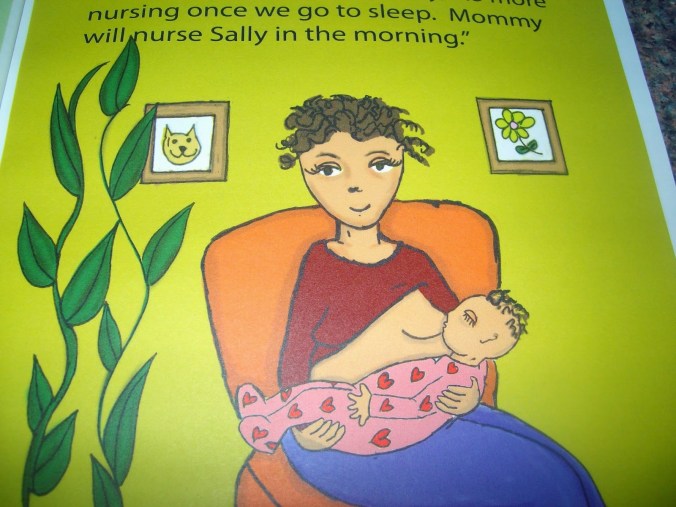
Lucy demonstrating her suggestion of bottle feeding near the breast.
Instead, parents can work on building in skin-to-skin contact. This may be through co-bathing, babywearing, baby massage etc. A lovely and easy way to get in regular and prolonged skin to skin is while feeding with the bottle. Mum can hold the bottle close to her breast and snuggle baby in close. This starts to rebuild the association that milk and breasts are related, and helps the parent to feel close and bonded to baby. When parents are feeling relaxed and close to their babies relactation tends to go a lot better. In fact, this is really important.
Here’s what tends to happen when someone wants to relactate: They are overwhelmed with guilt, shame, anger, confusion and grief for their experience of breastfeeding. The need to erase those feelings is so strong that they throw themselves into pumping, taking herbs, and demanding their GP prescribes Domperidone. And then, when things don’t happen quickly – they burn out and stop. They tell themselves they really can’t breastfeed, they have failed not once, but twice. That is potentially deeply damaging and we need to support families to avoid this happening.
When we instead focus on what parents actually miss about breastfeeding, we often learn that it boils down to the closeness.
We can recreate this with skin-to-skin contact and we can help Mum to learn that she is good and wise, and tuned into her Babe’s needs even without breastmilk. Once her healing here begins, the pumping won’t feel so desperate. She won’t be in such a hurry, won’t need quick results. She can think more clearly, be open to the idea that this might take many weeks, and that perhaps she will only be able to partially breastfeed until solids are introduced.
Once the hurt and grief are subsiding we can also begin to talk with the family about how breastfeeding is only a tiny bit about nutrition, and perhaps the breast/chest can become a lovely safe, relaxing space for reassurance, sleep and pain relief. Skin-to-skin – it’s my number one recommendation for relactation.
While Mum is rediscovering close, physical connection with her baby she can begin to rebuild her supply. A good breast pump isn’t essential, but if it’s an option then it will most likely make the process quicker. Mum needs to be pumping as close to 8x a day as she can manage, never going longer than 6 hours between pumping sessions. 15-20 minutes each breast is about right in the early days, finishing up with 5 minutes of hand expression. Generally, drops are seen quite quickly – days rather than weeks. The key here is consistency though. The breasts must be stimulated often to keep prolactin high and to keep the growing milk supply flowing so the breasts replace what’s been removed plus a bit more.
I firmly believe that our role as breastfeeding practitioners here isn’t to pressure the parent into expressing a certain number of times each day but to support them to find ways to pump as often as they feel able.
We can talk about putting baby in a bouncy chair which can be rocked with a foot while pumping, we can suggest roping in friends and family to hold baby, bring meals, run through a load of laundry, look after older siblings. We can encourage pumping to be seen as a chance for the parent to put their feet up with a favourite TV show or audio book. The list of creative ways to help pumping feel sustainable and less of a chore is endless.
Telling someone to pump every 2 – 3 hours for potentially several weeks, and then not helping that person find ways to achieve that goal is, in my opinion, unkind and only carrying out half a job.
The transition from bottle to breast needs to be carefully managed. As supply increases, the breast should be offered at regular intervals (no more than once every few days until baby is willing to latch, and once baby is happy at the breast, it can be offered before and after bottle feeds, or any time that just feels good) and pump afterward. Paced bottle feeding may give baby opportunity to show satiety cues and avoid overfeeding as they take more from the breast, but evidence to support this is woefully lacking. Frequent weight checks with a breastfeeding-friendly provider are very important and responding to any drop in centiles with an increase in supplements and pumping will protect Mother and baby as they work through this tricky part of their journey.
This is the point parents often begin to worry they can’t make enough milk, so they need a lot of emotional support as well as education around normal feeding behaviour and signs that baby is getting enough to help them transition to full breastfeeding and maintain it long term.
Gentle, empathic, positive care, focusing on how incredible mum is, how well her baby is growing, how dedicated she is, how connected to her baby she is etc., will all help bolster confidence in herself, her baby, and her body.
I can’t emphasize enough the importance of counseling and listening skills when dealing with a family wanting to relactate. These parents are often hurting intensely and are vulnerable to PND and low self-esteem. Relactation can be a powerful way to empower a family, and the correct support can genuinely facilitate that and change lives.
Are you a lactation specialist or one who is aspiring-to-be who has a special interest in a lactation-related topic? Perhaps you’d like to share your experience in the lactation field– tips, helpful resources, lessons learned, do’s and don’ts, challenges, etc. Or maybe you just have a lot to say! And that’s ok. Galactablog welcomes guest posts on a wide array of lactation-related topics. Contact us here or at galactablog{at}gmail{dot}com to share your ideas or for more information.

 Guest Post by Lesli Mitchell, MSW
Guest Post by Lesli Mitchell, MSW












 Are you a lactation specialist (of any kind) in private practice? Consider sharing your experience – tips, lessons learned, do’s and don’ts, challenges, etc. in Galactablog’s “Words from the Wise” series. Contact us
Are you a lactation specialist (of any kind) in private practice? Consider sharing your experience – tips, lessons learned, do’s and don’ts, challenges, etc. in Galactablog’s “Words from the Wise” series. Contact us 
 Are you a lactation specialist (of any kind) in private practice? Consider sharing your experience – tips, lessons learned, challenges, etc. in Galactablog’s “Words from the Wise” series. Contact us
Are you a lactation specialist (of any kind) in private practice? Consider sharing your experience – tips, lessons learned, challenges, etc. in Galactablog’s “Words from the Wise” series. Contact us 

 Are you a lactation specialist (of any kind) in private practice? Consider sharing your experience – tips, lessons learned, do’s and don’ts, challenges, etc. in Galactablog’s “Words from the Wise” series. Contact us
Are you a lactation specialist (of any kind) in private practice? Consider sharing your experience – tips, lessons learned, do’s and don’ts, challenges, etc. in Galactablog’s “Words from the Wise” series. Contact us 


 Are you a lactation specialist (of any kind) in private practice? Consider sharing your experience – tips, lessons learned, challenges, etc. in Galactablog’s “Words from the Wise” series. Contact us
Are you a lactation specialist (of any kind) in private practice? Consider sharing your experience – tips, lessons learned, challenges, etc. in Galactablog’s “Words from the Wise” series. Contact us 







 If you have a special topic that you’re passionate about – consider writing a Guest Post. I’d love to feature it and of course, give you all the credit. Plus, you’ll have a free opportunity for shameless self-promotion. Send me your ideas
If you have a special topic that you’re passionate about – consider writing a Guest Post. I’d love to feature it and of course, give you all the credit. Plus, you’ll have a free opportunity for shameless self-promotion. Send me your ideas  free breastfeeding-related videos for parents and professionals. All are free resources you can use to further your own lactation knowledge and to help those around you breastfeed. Galactablog is also on
free breastfeeding-related videos for parents and professionals. All are free resources you can use to further your own lactation knowledge and to help those around you breastfeed. Galactablog is also on  Galactablog is the ONLY blog in the world to publish reviews of lactation training programs in the weekly ‘Sunday Review’ series, so for those of you who’ve taken these trainings and/or finished lactation training programs, consider writing a
Galactablog is the ONLY blog in the world to publish reviews of lactation training programs in the weekly ‘Sunday Review’ series, so for those of you who’ve taken these trainings and/or finished lactation training programs, consider writing a